Avoid Becoming A Bully Massage Therapist
He pulled me to the side and I was immediately uncomfortable.
It used to happen all the time. One of my friends dad when I was growing up was a bully.
He was REALLY old school and believed that he was always right. It didn’t matter if he was blatantly wrong.
The worst part was when he would force his opinion on you and expect you to respect whatever his opinion was. He would regularly use intimidating factors to push his way around, especially if you ever had the nerve to question him.
Then the day came that I had enough.
When he pulled me aside that day, we were at a graduation party in a different town and he didn’t like the environment and the way other people were conducting themselves.
The reality is he just didn’t understand their culture so that made it wrong in his eyes.
However, he was going to enforce his opinion and demand this group of people change their behaviour and do what he thought was appropriate. The worst part was, he wanted me to go tell them to change, he didn’t want to do it himself.
I got my back up and wanted to go toe to toe with him (except he was way bigger and I don’t know how to fight). When I told him I wouldn’t have anything to do with it, he got angry and I mean really angry. He got in my face and looked at me saying “I’m a parent, not you, what I say goes”.
I had to put my foot down and tell him he could do whatever he wanted, but I would have no part of it.
A Balance Of Power
In this case there was a major imbalance of power.
This guy thought he had the right to impose his opinion on not only me, but every other person who was at this graduation party.
The problem is, he was blatantly wrong.
According to bullyingstatistics.com these type of people use their strength or position to harm, control and manipulate others, especially when those others have a difficult time defending themselves.
Do we consider this when we are dealing with our patients? Is there a balance of power there?
According to the College of Physical Therapists of BC “There is an inherent power imbalance in favour of the physical therapist, because the physical therapist has a disproportionate amount of knowledge compared to the patient, and the patient relies upon the therapist for care”
When we have a patient on our table we have to be careful of our communication and whether we are expressing opinions or fact. The two could be easily misinterpreted.
We must not impose our opinions on our patients.
It’s not only wrong, it’s against our ethics as Massage Therapists and healthcare professionals.
We see a variety of patients every day who walk into our clinics, some of us see a new person everyday, especially when we are trying to build our practice. Regardless of your background each one of the people who come to see you have a different background or come from a different culture that you may or may not be familiar with.
Whether we disagree with their lifestyle, religion, sexual orientation or anything else, we are medical professionals that must treat each person the same regardless of our opinion.
This also applies when speaking to them about other healthcare practitioners. We have to choose our words carefully.
We have all wanted to look at a patient and say “well your doctor is an idiot” but again this would be expressing an opinion, which could be potentially damaging to not only our relationship with the patient, but the relationship they have with other practitioners.
Remember the patient relies on us for care, not our opinion.
Applying Research
Staying up to date on research can be a difficult road to navigate.
Quite often it is going to challenge some long standing beliefs we’ve had, which can also change the way we treat and our relationship with a patient.
However it is part of our responsibility as healthcare professionals.
I saw a quote on Facebook the other day where someone said they had lost the passion for their practice because research has proven a technique they loved wrong. This could be debilitating for some, especially when we are talking about some long standing beliefs.
It is important to understand that the technique hasn’t necessarily lost its effectiveness, but our explanation of what is happening has to change. If our understanding has changed and we don’t relay the information to our patient this could be considered a form of harm.
Our patients look to us to stay informed and assume that we are doing everything in our power to provide quality care.
With so much information readily available to us nowadays we should be able to find a few ways to incorporate research into our practice for the benefit of our patients.
Whether it’s via Facebook groups, blogs or just searching for research online we should be making this part of our regular practice.
Take some time and check out a couple of blogs and websites. A few that I like are painscience.com, the international journal of therapeutic massage and bodywork, pubmed.com and rmtedu.com which all have some great information on various areas of research and evidence based resources.

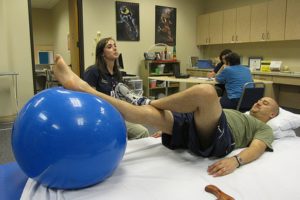
Photo by: Foundry
Communication Outside The Treatment Room
“If I wasn’t standing there, they would have had my daughter booked in once a week for the next two months!”
When I hear things like the statement above I think a little piece of me dies inside.
There is a drastic difference between a treatment plan and fear mongering.
Telling patients that they must come in for extended periods of time, without even knowing how a person will react to your treatment is a bullying tactic and it has to stop.
So does using terms like “well I only have one spot left, so you better take it before it’s gone”.
I get it, we all want a full practice but trying to tell someone you know how their body will be reacting two months down the road isn’t a treatment plan, it’s ego.
A proper treatment plan involves continual assessment and re-assessment to gauge progress.
As we move towards a patient centered healthcare system, these choices will more and more be the patients decision. Laying out a sound treatment plan and then incorporating the patient as part of the decision is how we will gain more respect in our medical community.
A patient should never feel pressured in making their healthcare decisions. We have to remember, even though it may not seem like it, there is a balance of power between us and our patients. We have responsibilities not only with our treatment but also in the way we communicate. Using any kind of communication where a patient feels pressured to book back in is an abuse of that power differential. As we strive to be more a part of mainstream healthcare all of these factors come in to play. Staying on top of relevant research can be intimidating but it improves not only our relationship with patients but also with other healthcare practitioners. It is our duty to stay informed and keep our patients informed so they can make the best decision for their healthcare. Just make sure you’re never in a position where a patient has to put their foot down with you.